Health Care Services
Normal And Cesarean Delivery
Vaginal Delivery/Normal Delivery
The natural, most common and safest method of childbirth is the vaginal delivery. In many cases, the delivery does not require any major intervention by the doctor. However, sometimes the gynaecologist/obstetrician may use special instruments like forceps (similar to large spoons) to guide the movement of the baby through the birth canal by cupping the head. Alternately, suction cup may be used, if required, to gently pull the baby out from the birth canal.
Cesarean Birth /C-section / Cesarean Delivery
Sometimes, a vaginal delivery may not be possible because of some complications. In such cases, the obstetrician conducts the delivery surgically, by making a cut in the belly of the mother and the uterus. Cesarean section nowadays is a commonly conducted and safe procedure. In most cases, a C-section doesn’t require general anaesthesia and epidural or spinal anaesthesia (an injection in the lower back where only the lower portion of the body is numbed) is adequate. A C-section is carried out by a trained obstetrician, with the help of an anaesthetist and trained nursing and operation theatre staff. Generally, a neonatologist also attends the procedure.
When is a Cesarean section advised?
A Cesarean section is advised as a planned mode of delivery in case some issues are identified beforehand. Some of the reasons include:
- Position of the baby is not as expected around the due date, i.e., head down.
- Medical issues with the mother which may be risky for the mother or the baby like, heart disease, infections, etc.
- Multiple pregnancy or more than one baby (twins or triplets).
- Previous history of Cesarean section which doesn’t allow a vaginal delivery to be attempted.
However, in many cases, a decision to undertake Cesarean section may be taken while the patient is in labour pain. Such unplanned Cesarean section is advised due to reasons such as:
- Risk to the baby by a peculiar positioning of the placenta or the umbilical cord
- Signs of distress of the baby like a very fast or slow heart rate
- Slow, hard labour
Labor Analgesia(Painless Labour)
Regional analgesia has become the most common method of pain relief used during labor in the India. Epidural and spinal analgesia are two types of regional analgesia. With epidural analgesia, an indwelling catheter is directed into the epidural space, and the patient receives a continuous infusion or multiple injections of local anesthetic. Spinal injections are usually single injections into the intrathecal space. A combination of epidural and spinal analgesia, known as a walking epidural, also is available. This technique combines the rapid pain relief from the spinal regional block with the constant and consistent effects from the epidural block. It allows sufficient motor function for patients to ambulate. Complications with regional analgesia are uncommon, but may include postdural puncture headache. Rare serious complications include neurologic injury, epidural hematoma, or deep epidural infection. Regional analgesia increases the risk of instrument-assisted vaginal delivery, and family physicians should understand the contraindications and risks of complications. Continuous labor support (e.g., doula), systemic opioid analgesia, pudendal blocks, water immersion, sterile water injections into the lumbosacral spine, self-taught hypnosis, and acupuncture are other options for pain management during labor.
Infertility Treatment
What is infertility?
What is infertility? Infertility is when you have trouble getting pregnant or staying pregnant. Fertility problems can happen in people of all genders, and can have many causes.
Infertility is common.
Some people have a hard time getting pregnant or staying pregnant. You’re generally diagnosed with infertility if you don’t get pregnant after 1 year or more of trying, or if you have multiple miscarriages. There are treatments for many kinds of infertility, and many people go on to have a healthy pregnancy and a child.
Fertility isn’t just a “woman’s problem” or an issue with age. Lots of things can lead to infertility, and it can affect people of all sexes and ages. When a couple has a hard time getting pregnant, either person (or both people) is equally likely to be the cause. That’s why both people are usually tested for infertility if a couple is having trouble getting pregnant.
What causes infertility?
Causes of infertility in cis women.
Some common reasons for infertility in cis women include:
- untreated chlamydia or gonorrhea
- not ovulating (not releasing eggs from your ovaries)
- your fallopian tubes are blocked so sperm can’t get to your egg
- poor egg quality
- the shape of your uterus makes it hard for a fertilized egg to implant
- endometriosis
- uterine fibroids
Cause of infertility in cis men
If you’re trans and using hormones
Gender affirming hormone treatments and surgeries can lead to infertility, but they don’t always lead to infertility. If you want to get pregnant, talk with your doctor or nurse about your fertility options. If you don’t want to get pregnant, use birth control.
What might increase my risk of infertiliy?
There are certain health and lifestyle factors that can increase your chances of having fertility problems. They include:
- being older than 35 (for women)
- being very overweight or underweight
- chemotherapy or radiation
- lots of exposure to environmental toxins, like lead or pesticides
- excessive drug or alcohol use
- smoking cigarettes
- not getting recommended testing for chlamydia/gonorrhea
- a history of pelvic inflammatory disease (PID)
- injury to the scrotum and testes
- overheated testicles (from wearing clothing that’s too tight, or swimming or bathing in hot water often and recently)
- having an undescended testicle
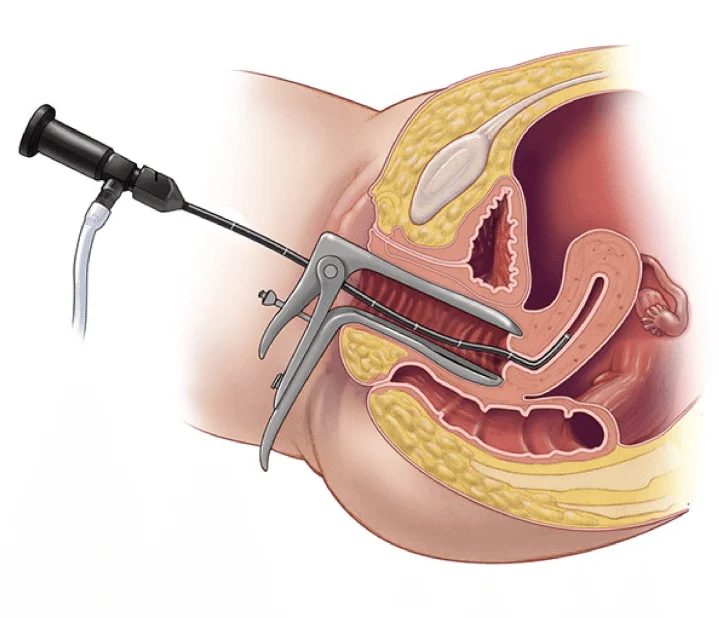
To evaluate the outside portion of the uterus, fallopian tubes, ovaries, and internal pelvic area always the diagnostic laparoscopy is recommended or done,and the same is used to look inside the uterus also. If any abnormalities detected during the diagnostic procedure, one of the operative procedure can be performed to correct it at the same time and also avoids the need for a second surgery.
In this department, all laparoscopic surgeries are being carried out, like
- Appendix
- Ovarian drilling
- Diagnostic laparoscopy for infertility patients
- Cholecystectomy
- Fertility enhancing endoscopic surgeries like myomectomy, ovarian cystectomy, tubal canalisation.
- Total laparoscopic hysterectomy
- Laparoscopic Adhesiolysis
- Hysteroscopic Procedures like Myomectomy, Septal Resection, Adhesiolysis and Lateral Metroplasty
High Risk Pregnancy Managment
Pregnancy and birth are natural processes. Most pregnancies are low risk-healthy mom, healthy baby, no complications. When your not underweight or overweight, with no chronic health issues, age less than 35 years and if you are most likely to go through a safe pregnancy and birth. Today , 88% of pregnancies have a physiological course which needs just basic care, while 12% of cases are of the higher-risk category that requires addintional care.
So what is high risk pregnancy?
High risk means that you or your baby’s life could be at a risk of complications.
It can be the result of a medical condition present before pregnancy or a medical condition that develops during pregnancy. For example, if you are carrying more than one baby it is called a multiple pregnancy or if the baby has some developmental issues either of you can be at risk. While all pregnancies can be challenging, high risk pregnancies can possess significant challenges to the health of both the mother and the fetus.
What are the risk factors ?
There are various risk factors for pregnancy. Specific factors that might contribute to a high-risk pregnancy include:
- Advanced Maternal Age :
Surveys have revealed that in the last few years much risk is attributable to the increase in the average age of women who get pregnant . Pregnancy risks are higher for mothers age 35 and older.
- Lifestyle Choices :
Tobacco use including smoking, alcohol consumption and drug abuse could put a pregnancy at risk.
- Medical History :
A prior C-section, a previous low birth weight baby or preterm birth — birth before 37 weeks of pregnancy — might increase the risk in subsequent pregnancies. Other risk factors include a family history of genetic conditions, a history of pregnancy loss or the death of a baby shortly after birth.
- Underlying Conditions :
Chronic conditions — such as diabetes, high blood pressure and epilepsy — increase pregnancy risks. A blood condition, such as anemia, an infection or an underlying mental health condition can also increase pregnancy risks.
- Pregnancy Complications :
Various complications that develop during pregnancy pose risks, such as problems with the
- uterus, cervix or placenta.
- Other concerns might include too much amniotic fluid (polyhydramnios) or low amniotic fluid (oligohydramnios).
- Restricted fetal growth, or
- Rh (rhesus) sensitization — a potentially serious condition that can occur when your blood group is Rh negative and your baby’s blood group is Rh positive.
- hypertension.
- diabetes, or
- infectious diseases
- Multiple Pregnancy :
Pregnancy risks are higher for women carrying twins or higher order multiples.
Risk factors for pregnancy also involve fears and anxieties that make the gestation period more stressful.
Steps to be taken to go through a healthy pregnancy
High risk pregnancies require more advanced level of pregnancy consultation and monitoring as they carry huge risk of complications and problems for a baby’s health at the time of birth and beyond. Women with high risk pregnancies will have to be counseled by a high risk pregnancy specialist to be specifically attentive toward their health, have a nutritious diet, maintain proper amount of weight and avoid the consumption of any risky substances or medications. Regular prenatal visits, regular maternal and fetal screening as well as additional prenatal tests are usually recommended to further assess the health and development of the baby. Delivery of a high risk pregnancy is better to take place in a well equipped hospital setting, under the guidance of a good obstetrician.
Medical & Surgical Termination of Pregnancy
Reasons to Choose a Suction Curettage (Surgical) Abortion
Contraceptive Advice
FEMALE CONTRACEPTION
MALE CONTRACEPTION
Cervical Cancer Screening
What is cervical cancer?
What causes cervical cancer?
Most cervical cancers are caused by Human Papillomavirus (HPV) infections. HPV is a group of viruses that are extremely common worldwide. There are more than 100 types of HPV, of which at least 14 are cancer-causing (also known as high risk types). Two HPV types (16 and 18) cause 70% of cervical cancers and pre-cancerous cervical lesions. There is also evidence linking HPV with cancers of the anus, vulva, vagina, penis and oropharynx.
Sonography & Fetal Medicine
Fetal Medicine
Pregnancy comes with a mixture of emotions and millions of questions. The responsibility of your baby growing within you is great, yet the the outcome is to be treasured.
The journey to becoming a parent is not easy, and it can be overwhelming! That is why every pregnant mother is very aware of and curious to know about the well-being of her child. So hang in there, mama! You are not the only one to wonder about what is happening and what is to come in the near future.
Technology has revolutionized the world of healthcare and has provided answers to the expectant mothers out there. It has catered answers to all the inquisitive families about the growing baby’s health, development and more. Yes, with the help of ultrasound you can know the health of the growing baby inside you.
What is an ultrasound?
Ultrasound is a type of imaging technique that uses harmless high-frequency sound waves rather than radiation to look at structures and organs inside the body.
What is pregnancy ultrasound?
A pregnancy ultrasound is used to check the health of the baby and the mother’s reproductive organs.
It is also known as a sonogram. Here the doctor or the healthcare specialist monitors the fetal development and checks if there are any potential problems or threat.
With the advancement in technology, along with a standard one, there are many different types of ultrasounds. They are:
- 3-D ultrasound :
A 3-D ultrasound gives three-dimensional details of the growing baby. It allows your doctor to see the width, height, and depth of the fetus and the mother’s organs. The 3-D ultrasound follows the same procedure as the standard 2-D ultrasound but uses a unique probe and software to craft the 3-D image.
3-D ultrasound is very helpful in finding out any suspected problems during the pregnancy. - 4-D ultrasound :
A 4-D or a dynamic 3-D ultrasound is similar to the standard 3-D ultrasound, but it creates a moving video of the fetus with better resolution of the baby’s face and movements.
- Transvaginal ultrasound :
A transvaginal ultrasound is used during the early stages of pregnancy to get more resolution in the image captured (more precise than the standard ultrasound) of the growing fetus. It is named so because a small ultrasound probe is inserted into the vagina (rests against the back of the vagina) while the images are being taken.
- Fetal echo-cardiography :
Fetal echo-cardiography is performed to look into the details at the fetus heart (heart’s size, shape, and structure). It is suggested if your doctor suspects any congenital heart defects and to find out how your baby’s heart is functioning.
What to expect while undergoing an ultrasound?
An ultrasound test is a very simple procedure. Once you meet the technician/ doctor, you are asked to lie on a table straight facing upward. A gel is applied to the lower abdominal region. The gel acts as a conductive medium which makes the bond between the skin and the probe or transducer stronger. Then he/she moves the transducer over the part of your body. The transducer transfers sound waves which bounce off the body tissues and captures the wave that bounces back creating an image from the sound waves.
Is pregnancy ultrasound safe?
Yes, completely! A recent study confirms that multiple ultrasound examinations during pregnancy do not cause any harmful lasting effect to the developing fetus. It is a safe and accurate way to keep track of the health of your growing little one.
Therefore, a regular doctor’s check-up is a must for you and your bundle of joy!

